An
extensive amount of research has been conducted on the effects of massage
therapy. Research data has shown that massage produces measurable biological
effects and may have an effect on the immune system.[1]
While some of this scientific evidence is preliminary it has shown that massage
can also help with back pain, neck pain, headaches, extremity pain and may
improve quality of life for people with depression, cancer, HIV/AIDS and when
utilized appropriately and provided by a trained professional, massage therapy
appears to have few risks.[2]
Massage
therapy focuses on the muscle and other superficial soft tissues of the body to
help alleviate tension, inflammation, and pain via the application of manual hands-on
techniques. The goal of massage is to establish and maintain good physical
condition and health by normalizing and improving muscle tone, promoting
relaxation, stimulating circulation, and producing therapeutic effects on the
respiratory and nervous systems.[3]
So what is massage therapy?
Swedish
massage utilizes long strokes, kneading, deep circular movements, vibration,
and tapping.
Deep
tissue massage focuses on certain painful, stiff "trouble spots" in
your body and utilizes slow, deliberate strokes that focus pressure the
muscles, tendons, or other tissues deep under your skin and provides relief
from chronic patterns of tension and injuries such as back sprain.[4]
Structural
massage, also known as myofascial release, manipulates the soft tissues within
the body using different angles and degrees of physical pressure to stretch and
guide fascia to a place of easier movement.[5]
Research has shown that this style of massage produces positive effects on
pain, anxiety, depression, fatigue, and stiffness in those suffering with
fibromyalgia.[6]
Myofascial trigger point therapy is most effectively utilized in the treatment of chronic
and acute pain. Postural holding patterns, emotional stresses and work-related
muscular usage all contribute to areas of contracted muscle that develop firm
nodules or taut bands know as trigger points which most of the time we aren’t even
aware of. When pressed, trigger points are painful and are associated with pain
elsewhere in the body and without direct intervention to eliminate them will
not go away on their own.[7]
So
what exactly does medical research say about massage?
Since
2008, the National Center for Complementary and Integrative Health (NCCIH) a
division of the U.S. Department of Health & Human Services has taken an
active role in not only reviewing the available literature but has also funded clinical trials on massage therapy. This is what they have discovered:
-
Massage therapy helped reduce pain, improve function, and decrease the use of
anti-inflammatory medication more effectively than usual medical care[8]
in people with chronic low-back pain.[9]
- Massage
therapy led to statistically significant improvements in neck pain severity,
pain-related disability and function, and in one study participants reported a
14% decrease in the use of pain medication.[10]
[11]
- A
2012 study found that a 60 minute massage once per week exhibited significant
improvements in pain, function, and global response compared with those
receiving usual care medical care for osteoarthritis of the knee.[12]
Aside
from the research conducted by the NCCIH there have been other studies that
have found myofascial therapy to also be an effective form of treatment for
conditions such as tension type headache [13]
[14]
[15]
[16],
temporomandibular joint (a.k.a. TMJ) pain[17],
and chronic shoulder pain.[18]
Chronic
muscular restriction can inhibit essential physiologic processes such as blood
flow, lymphatic drainage, nerve conduction, and cellular metabolism which can,
over time, affect our overall health. The primary reason for the therapeutic
effects of massage therapy is that it increases blood flow in small vessels that
has been impeded due to muscle tension and that leads to better and faster
recovery around the muscle tissue which in turn improves the range of motion,
reduces swelling, and has pain-reducing properties.[19]
[20]
Dr.Sean Konrad at Life in Motion Chiropractic and Wellness applies a collection of
skills when performing therapeutic myofascial treatment, however the type of therapy
performed will depend on your needs and physical condition.
 |
| Chair Massage |
or on a flexion-distraction therapy table for cases in which a more deep tissue approach is warranted.
Aside from this he can also apply a range of modalities to supplement this hands-on therapy which include:
 |
| Heat or Ice Application |
 |
| Muscle Stimulation |
 |
| Hot Stone Massage |
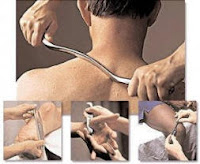 |
| Instrument Assisted Soft Tissue Manipulation |
 |
| Kinesio Tape Application |
Here a short summary of Dr. Konrad’s formal training in myofascial techniques:
[1] Rapaport
MH, Schettler P, Bresee C. A preliminary study of the effects of a single
session of Swedish massage on hypothalamic-pituitary-adrenal and immune
function in normal individuals. (http://www.ncbi.nlm.nih.gov/pubmed/20809811)
The Journal of Alternative and Complementary Medicine. 2010; 16(10):1–10.
[2] Field,
Tiffany, PhD, Andrea Furlan, MD, Karen Sherman, PhD, Partap Khalsa, DC, and
John Killen, MD. "Massage Therapy for Health Purposes." National
Center for Complementary and Integrative Health. U.S. National Library of
Medicine, 06 Sept. 2016. Web. 21 Sept. 2016.
[3] Fritz,
Sandy. "Chapter 2." Mosby's Fundamentals of Therapeutic Massage. 4th
ed. St. Louis, MO: Mosby/Elsevier, 2009. 30-33. Print.
[4] Keifer,
David, MD. "Massage Therapy Styles and Health Benefits." WebMD.
WebMD, 01 Aug. 2016. Web. 21 Sept. 2016.
[5] Konopelky,
Karin. "Structural Integration." Massage Therapy 101. Tsavo Media
Canada Inc., n.d. Web. 22 Sept. 2016.
[6]
Yuan SL, Matsutani LA, Marques, AP. Effectiveness of different styles of
massage therapy in fibromyalgia: a systematic review and meta-analysis. Man Ther. 2015;(2):257-264
[7] Finando,
Donna. "What Is the Difference Between an Acupoint and a Trigger Point?
Part 1." MASSAGE Magazine. Massage Magazine, 08 Dec. 2008. Web. 01 Mar.
2017.
[8]
Usual care for low-back pain may include medication, other forms of physical
therapy, back exercises, and education.
[9]
Cherkin DC, Sherman KJ, Kahn J, et al. A comparison of the effects of 2 types
of massage and usual care on chronic low-back pain: a randomized,
controlled trial. (http://www.annals.org/content/155/1/1.abstract?aimhp) Annals
of Internal Medicine. 2011;
155(1):1–9.
[10]
Sherman KJ, Cherkin DC, Hawkes RJ, et al. Randomized trial of therapeutic
massage for chronic neck pain. Clinical Journal of Pain. 2009; 25(3):233–238.
[11] Sherman
KJ, Cook AJ, Wellman RD, et al. Five-week outcomes from a dosing trial of
therapeutic massage for chronic neck pain.
(http://www.ncbi.nlm.nih.gov/pubmed/24615306) Annals of Family Medicine.
2014;12(2):112–120.
[12]
Perlman AI, Ali A, Njike VY, et al. Massage therapy for osteoarthritis of the
knee: a randomized dose finding trial. PLoS One. 2012; 7(2):e30248.
[13] Doraisamy,
Magesh Anand, Charles Prem Kumar & Anshul, and Chandran Gnanamuthu.
"Chronic Tension Type Headache and the Impact of Myofascial Trigger Point
Release in the Short Term Relief of Headache." GJHS Global Journal of
Health Science 2.2 (2010): 239-44. Web.
[14] Fernández-De-Las-Peñas,
César, and Carol A. Courtney. "Clinical Reasoning for Manual Therapy
Management of Tension Type and Cervicogenic Headache." Journal of Manual
& Manipulative Therapy 22.1 (2013): 45-51. Web.
[15] Quinn,
Christopher, Clint Chandler, and Albert Moraska. "Massage Therapy and
Frequency of Chronic Tension Headaches." American Journal of Public Health
92.10 (2002): 1657-661. Print.
[16] Ferna´ndez-de-las-Pen˜
as, Cesar, Maria L. Cuadrado, and Juan A. Pareja. "Myofascial Trigger
Points, Neck Mobility, and Forward Head Posture in Episodic Tension-Type
Headache." Headache 47 (2007): 662-72. Print.
[17] Miernik,
Marta, Mieszko Więckiewicz, Anna Paradowska, and Włodzimierz Więckiewicz.
"Massage Therapy in Myofascial TMD Pain Management." Advances in
Clinical and Experimental Medicine 21.5 (2012): 681-85. Print.
[18] Bron,
Carel, Arthur De Gast, Jan Dommerholt, Boudewijn Stegenga, Michel Wensing, and
Rob Oostendorp. "Treatment of Myofascial Trigger Points in Patients with
Chronic Shoulder Pain: A Randomized, Controlled Trial." BMC Medicine.
BioMed Central Ltd., 24 Jan. 2011. Web. 30 Jan. 2017.
[19] Goats
GC: Massage – the scientific basis of an ancient art: part 2. Physiological and
therapeutic effects. Br J Sp Med 1994, 28(3), 153–156.
[20] Smith
AR Jr.: Manual Therapy: The Historical, Current, and Future Role in the
Treatment of Pain. Sci World J 2007, 7, 109–120.




