 |
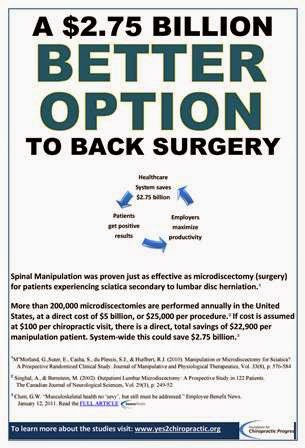
| Better Option to Back Surgery |
“The American Association of
Medical Colleges has identified musculoskeletal medicine as an area in which
students receive inadequate
preparation for practice in
the real world.[1]
North American medical schools have limited time devoted to musculoskeletal
education. Only 30% to 40% of schools have required instruction in the
musculoskeletal system.[2][3]
Graduates entering practice experience the effects of this lack of instruction;
one survey found that half of family physicians reported inadequate
musculoskeletal training for clinical practice.[4]”[5]
These are not the words of an opinionated
and/or biased chiropractor but those of clinical researchers at the University
of Rochester School of Medicine and Dentistry. They admit that as of November 2014,[5] most primary care physicians graduating
from medical school lack the confidence to assess and treat musculoskeletal
complaints. This fact alone creates a substantial argument for the necessity of
an integrative system of healthcare delivery that incorporates Primary
Spine Practitioner (PSP) trained providers who possess the knowledge,
skill, and ability to triage[6]
patients with musculoskeletal complaints.
PSP trained providers [DC, PT,
MD, NP, PA] can evaluate and manage the majority of patients with
musculoskeletal conditions based upon best available evidence, and in a patient
centered model of care. This portal of entry into the healthcare delivery
system can then streamline the referral process for those patients who need a
level of care beyond that of standard musculoskeletal treatment. Incorporating
this type of provider would alleviate the burden of musculoskeletal complaints
from primary care practices allowing medical doctors to focus on infectious
disease and serious pathology, conditions they ARE TRAINED FOR.
The desire for this integration became evident to us
upon receiving a letter from Excellus Blue Cross/Blue Shield of Rochester dated
29 December 2014. In this letter they outlined a “Waived Copayment Pilot
Program” whose purpose is to “help drive care to spine
pathway trained practitioners so that the program’s value can be measured
and compared to other modalities of treatment for back and neck pain”. This
program will extend until 31 December 2015 and only include Excellus employees
and their covered family members but underlines the fact that a major health insurer
believes PSPs are credible portal of entry providers for patients who
present with musculoskeletal conditions.
[1] Association
of American Medical Colleges. Medical School Objectives Project. Contemporary
issues in medicine: musculoskeletal medicine education. Report VII. 2005.
[2] DiCaprio
MR, Covey A, Bernstein J. Curricular requirements for musculoskeletal medicine
in American medical schools. J Bone Joint Surg Am. 2003 Mar;85(3):565-7.FREE
Full Text
[3] Pinney
SJ, Regan WD. Educating medical students about musculoskeletal problems. Are
community needs reflected in the curricula of Canadian medical schools? J Bone
Joint Surg Am. 2001 Sep;83(9):1317-20.Abstract/FREE
Full Text
[4] Sneiderman
C. Orthopedic practice and training of family physicians: a survey of 302 North
Carolina practitioners. J Fam Pract. 1977 Feb;4(2):267-50.Medline
[5] DiGiovann,
Benedict F., , MD, Richard D. Southgate, , MD, Christopher J. Mooney, , MA,
MPH, Jennifer Y. Chu, , MD, David R. Lambert, , MD, and Regis J. O’Keefe, , MD,
PhD. "Factors Impacting Musculoskeletal Knowledge and Clinical Confidence
in Graduating Medical Students."The Journal of Bone and Joint Surgery E185
96.21 (2014): n. pag. The Journal of Bone and Joint Surgery, Inc.
The Journal of Bone and Joint Surgery, Inc.; STRIATUS Orthopaedic
Communications, 05 Nov. 2014. Web. 17 Jan. 2015. <http://jbjs.org/content/96/21/e185>.
Investigation performed at the Department
of Orthopaedics and Rehabilitation, University of Rochester School of Medicine
and Dentistry, Rochester, New York
Link to the full article:


