The 24 vertebrae and interlaying discs of the spinal column
protect your bodies’ most important and delicate system, the central nervous
system, and impingements within the joints of your spinal column can contribute
to a number of health problems and ailments.
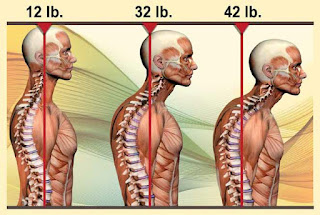
Over time the human body can and will experience static
malalignments that alter the optimal resting length and tension of the muscles
within the musculoskeletal system. Common static malalignments include joint
fixation and myofascial adhesions that lead to or can be caused by poor
posture.
- Poor posture and repetitive movements can create
dysfunction within the connective tissue of the human movement system
- This dysfunction is treated by the body as an injury and
will initiate a repair process termed the cumulative injury cycle
- Any trauma to the tissue of the body creates
inflammation. Inflammation in turn activates the body’s pain receptors and
initiates a protective mechanism, increasing muscle tension and causing muscle
spasm.
- These muscle spasms are not like a calf cramp. Heightened
activity of muscle spindles in particular areas of the muscle create, in essence,
a microspasm.
- As a result of the spasm, adhesions (“knots” or “trigger points”) will begin to form in the soft tissue. These adhesions form a weak,
inelastic (unable to stretch) matrix that decreases normal elasticity of the
soft tissue
- Left unchecked, these adhesions can begin to form
permanent structural changes in the soft tissue that are evident by Davis’s
law1 which states that soft tissue will model
along the lines of stress.
- Soft tissue remodels or rebuilds itself with an inelastic
collagen matrix that forms in a random fashion. This simply means that it
usually does not run in the same direction as the muscle fibers. If the muscle
fibers are lengthened, these inelastic connective tissue fibers are acting as
roadblocks, not allowing the muscle fibers to move properly. This creates
alterations in normal tissue extensibility and causes relative inflexibility
- Because of the large number of joints in the spine and
the tremendous demand upon the spine for motion, muscle contraction for
stabilization is particularly important, and when excessive, can result in
hypomobile joints.
Joint dysfunction (a.k.a. hypomobility) is one of the most
common causes of pain in the human body.
- The zygapophyseal, or facet, joints are complicated
biomechanical structures in the spine, with complex anatomy, mechanical
performance and effects on overall spine behavior and health.
- At each spinal level, there is a pair of facet joints
located on the postero-lateral aspects of each motion segment, spanning from
the cervical to the lumbar spine
- The facet joints, together with the intervertebral discs
and spinal ligaments, connect the adjacent vertebrae of the spine at all
regions and provide support for the transfer and constraint of loads applied to
the spinal column. These articulations insure the mechanical stability and also
overall mobility of the spine, while protecting the spinal cord running through
it.
- Joint dysfunction literally means “bad motion.” There are
two types of joint dysfunction: too little motion termed a hypomobility; and
too much motion termed a hypermobility.
- If motion is altered at any one joint level,
compensations usually occur at adjacent segmental levels to restore proper
motion of the spine. For this reason a hypomobility at one level usually
results in a compensatory hypermobility at an adjacent level, and vice versa.
These compensations can then leapfrog up (or down) the spine, creating entire
regions of dysfunction.
- The primary causes of spinal joint hypomobility can be
divided into three types: taut soft tissue, bony obstruction, and jammed
meniscoid body.
- Taut soft tissues and bony obstruction can be factors in
all joint dysfunction hypomobilities of the body. However, in the case of
spinal joints, a third cause of hypomobility has been proposed; that is a
meniscoid body that has become pinched and jammed between the surfaces of the
facet joint. A meniscoid body is a fibrous, fatty soft tissue that is located
at the periphery of a joint space. If it displaces and moves toward the center
of the joint, it can become pinched and swollen, obstructing motion toward that
side of the joint.
- The synovial folds, or meniscoids or menisci, are
intra-articular structures that protect the articular cartilage when opposing
articulating surface glide on each other during joint motion
- This protection is realized since the meniscoids
compensate for the incongruence of the joint's articular surfaces, guiding and
smoothing their relative motion, and distributing the load over a greater
surface area
In addition to these primary causes of joint hypomobility, a common secondary cause of hypomobile spinal joints is overuse due to compensatory hypermobility. When one segmental joint level is hypomobile, the adjacent joint will often become hypermobile to compensate so that the region still has full gross range of motion. In time, excessive motion at the compensatory hypermobile joint level can lead to overuse and irritation to that joint (in the parlance of Leon Chaitow: “used, overused, misused, abused”), thereby triggering muscle tightness to splint and stop its motion. Now there are two segmental hypomobile joints, causing the next adjacent joint level to become even more hypermobile to compensate. In time, this second hypermobility can also become overused and irritated, triggering muscle tightness and causing it to become hypomobile. In this manner, hypomobilities often spread through the spine. Because the musculature that tightens is often small intrinsic musculature, this condition is usually not symptomatic until the region of hypomobility is so great that full compensation by adjacent joints is not possible and gross range of motion decreases.
The longer a hypomobile joint or hypomobile region is
allowed to exist, the worse it becomes. Lack of motion allows for the continued
deposition of fascial adhesions that increasingly lock up the area. Allowing a
hypomobility to continue also allows the increased muscle tone of the region to
become more patterned into the nervous system. For these reasons, joint
hypomobility tends to be a progressive condition that expands in both intensity
and in scope throughout the spine. Indeed, it is not uncommon for middle aged
and elderly clients to have large regions of their spine locked in hypomobility.
The overall result is that once begun, this pattern of hypomobility
progressively worsens as we age.
Once a joint has lost its normal range of motion, the
muscles around that joint may tighten to minimize the stress at the involved segment
or become overactive to prevent movement and further injury. This process
initiates the cumulative injury cycle which subsequently alters normal movement
patterns and leads to structural and functional inefficiency.
The doctors at Life in Motion Chiropractic & Wellness
have been specifically trained to assess and treat joint dysfunction,
myofascial adhesions, as well as a variety of other musculoskeletal disorders.
The goal of treatment at Life in Motion Chiropractic and
Wellness is to restore balance, flexibility, and control which instills
self-efficacy and helps to keep your body moving naturally, feeling good, and
aging well.
To learn more visit us at LifeInMotionChiro.com
1: Davis's law is used in anatomy and physiology to describe how soft tissue models along imposed demands. It is the corollary to Wolff's law, which applies to osseous tissue. It is a physiological principle stating that soft tissue heal according to the manner in which they are mechanically stressed.